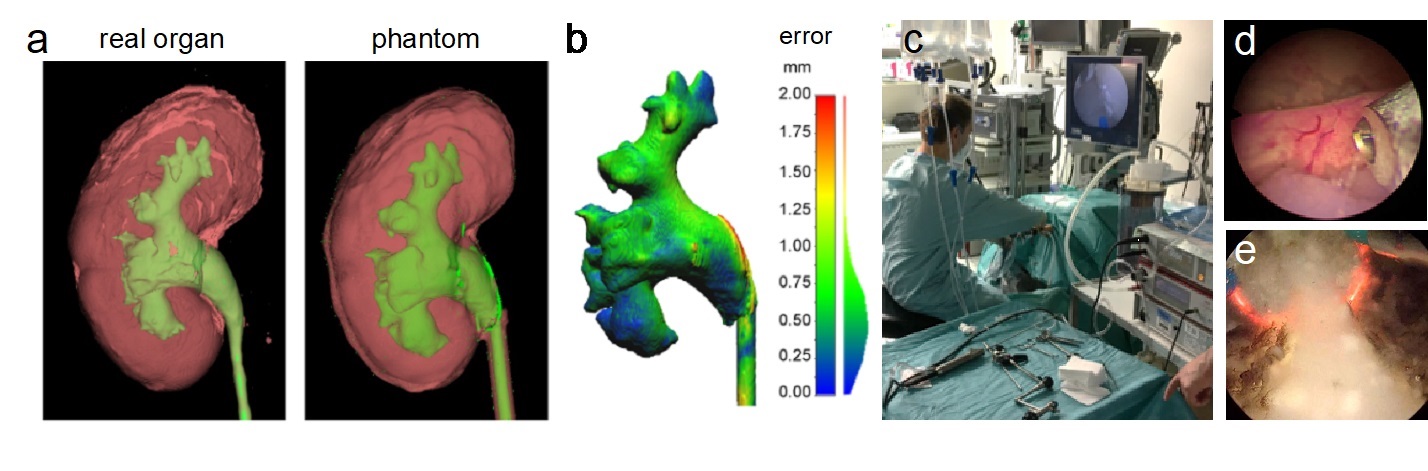
Realistic organ phantoms for medtech and surgical training. (a) CT scan of kidney phantoms showing the same anatomy as a human kidney. (b) 3D reconstruction of the collecting system shows high precision of the phantom with an average spatial error of only 0.5 mm. (c) A surgeon performs a surgery on our phantom in an operating theatre. (d-e) Several surgical procedures have been successfully simulated using our phantoms, including an endoscopic laser surgery (d), and electrocautery surgery (e).
Introduction and problem: The traditional way of surgical training – “see one, do one, teach one”— should be replaced by modern model-based surgical simulation. Models (phantoms) are safer for patients, offer a wider choice of disease models and a smoother learning curve. Animal models are often unrealistic and may be ethically problematic. Therefore, to train medical personnel, test new procedures, and to develop new medical instruments, realistic in vitro human-like organ models are needed. This is especially so for robotic surgery, where there is high demand for such technology. The challenge of making phantoms is that 3D printing materials are unsuitable (Young’s modulus) and most commercial models are too basic, with incorrect appearance and contrast in medical imaging, and do not offer a way to quantitatively assess the surgery.
Our approach: We combined our unique expertise in materials research and fabrication with the practical knowledge of our medical collaborators to build several organ models, including urinary tract models with bladder, kidney and prostate, as well as an aneurysm within a liver model. They are anatomically correct with fine 3D features, are made using from customized biomimetic soft materials that show the correct imaging contrast (optical, X-Ray, and ultrasound), and offer a realistic surgical response (e.g. when cut, sutured or cauterized). We have also patented a method that permits the quantitative assessment of the surgery using a second contrast agent and imaging modality.
Results: In collaboration with the medical teams, we validated the organ phantoms under realistic surgical conditions and demonstrated their usefulness in endoscopic, laparoscopic, and robotic surgeries. Our materials are mainly hydrogels with additives and behave like real tissue. Different imaging methods were used during and after the surgical simulation and in some cases this was combined with machine learning to provide quantitative feedback to the trainees. We published Multiple journal and conference papers based on this project [ ].
Discussion and outlook: We were awarded an ERC Proof of Concept grant and filed two patents (1 granted, 1 pending) to protect the technology. Major medical device companies have contacted us and one leading endoscope manufacturer will run their first training at an international conference in Canada using our phantoms. With the support from Max Planck Innovation GmbH, a spin-off is being prepared
